Management of Perioperative Bronchospasm
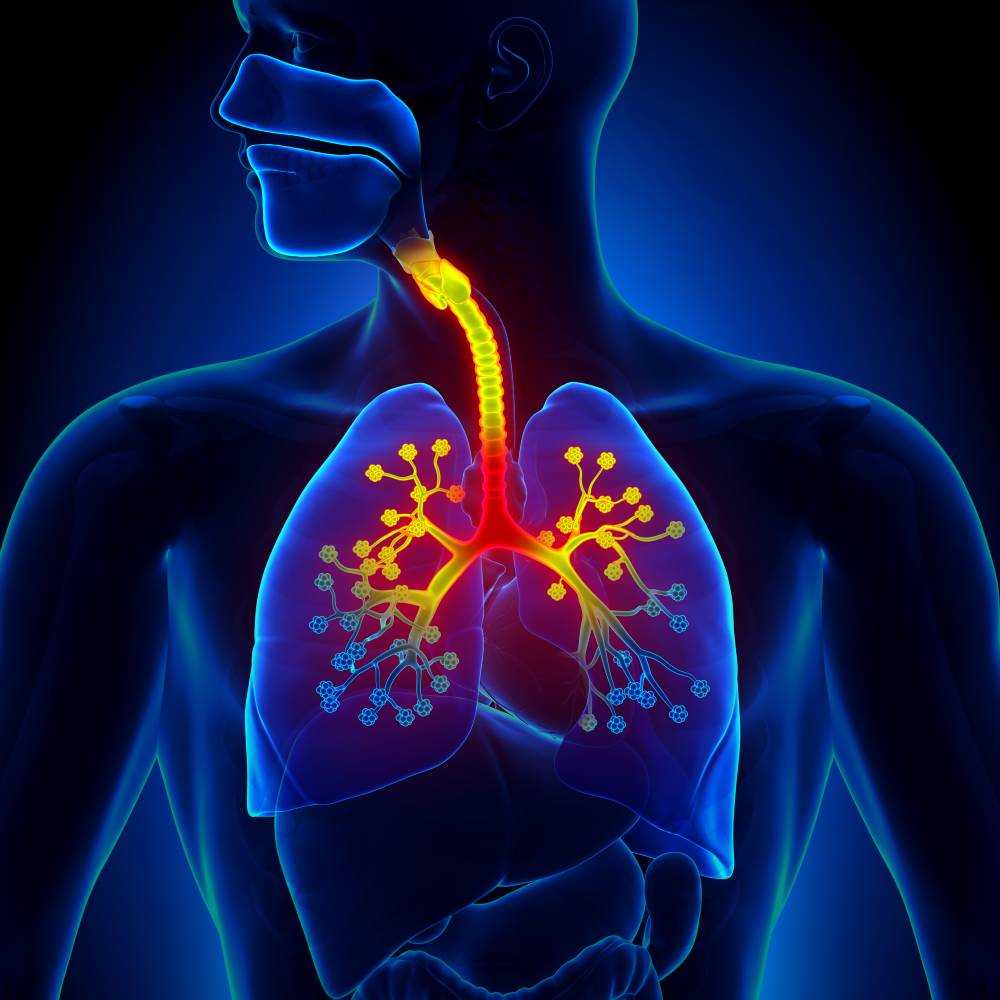
Bronchospasm involves the sudden constriction of muscles in the walls of bronchioles. This condition manifests as wheezing and shortness of breath. Its root causes include foods, medicines, other allergens, and hormone levels. Bronchospasm that occurs around the time of surgery, especially during anesthetic induction, is called perioperative bronchospasm (PB). To prevent severe injury or death, the anesthesia team must quickly identify and manage PB when it arises.
Some patients exhibit risk factors that can lead to PB, including asthma, heavy smoking, and chronic bronchitis [1][2]. For example, patients who experience asthma attacks several days before surgery are more susceptible to PB [3]. Similarly, young smokers (16-39 years old) and female smokers are more susceptible to PB than other smokers [1]. Although the research on PB risk factors is sparse, providers should draw on available medical knowledge to screen their patients for PB risk.
Medical research has also found that certain procedures are more likely to cause PB. For example, the unique characteristics of anesthetic induction and endotracheal intubation make PB especially prevalent. Situations like airway irritation, breathing tube misplacement, and pulmonary aspiration can trigger PB [1]. During the anesthetic maintenance stage, allergies are the most likely cause of PB, with endotracheal tube malposition and airway irritation as less likely causes [1]. A separate clinical study confirmed that PB correlates with endotracheal intubation and thoracic/abdominal surgeries [3]. During these procedures, medical providers should be ready to treat PB, especially among patients at higher risk in general.
A wide variety of pharmaceuticals exist to treat PB. One study describes two categories of PB treatment: acute therapy and chronic therapy [2]. Acute therapy covers pharmaceuticals for immediate treatment in the operating room, including parenteral corticosteroids, volatile anesthetic agents, and inhaled short-acting β-agonists. Chronic therapy addresses long-term maintenance to reduce the likelihood of PB, involving inhaled corticosteroids and leukotriene modifiers. Acute PB therapy is especially difficult because PB can quickly cause brain damage or death via hypoxia. Even if the necessary medications are on hand, providers must have an efficient workflow to choose and administer those medications. One study suggests the use of emergency manuals. In a crisis simulation and in the clinical setting, providers were able to complete necessary actions needed to treat PB with the use of an emergency manual, including the choice and sequence of certain acute therapies [4]. Another study suggests the use of novel delivery mechanisms for inhaled medications, especially for patients who are intubated or cannot breathe normally [5]. With practices like these, providers can help reduce the rate and severity of PB incidents.
Perioperative bronchospasm is relatively rare compared to other perioperative complications. One study found that, across thousands of closed medical claims, PB was mentioned in just two percent of cases [2]. However, of those cases, over ninety percent led to severe injury or death. These findings are consistent with assertions that PB is understudied in the medical research [1] and inadequately addressed in clinical settings [2]. Future research will likely develop more efficient workflows and medical equipment for acute PB therapy, as well as study the underlying mechanisms of PB across patient risk factors.
References
[1] P. Dewachter, et al. Case Scenario: Bronchospasm during Anesthetic Induction. Anesthesiology May 2011; 114. DOI:10.1097/ALN.0b013e3182172cd3.
[2] B. D. Woods, et al. Perioperative Considerations for the Patient with Asthma and Bronchospasm. British Journal of Anaesthesia 2009; 103. DOI:10.1093/bja/aep271.
[3] Y. Kumeta, et al. A Survey of Perioperative Bronchospasm in 105 Patients with Reactive Airway Disease. The Japanese Journal of Anesthesiology 1995; 44: 3. PMID:7745793.
[4] J. Huang, et al. The Use of Emergency Manuals Leading to Successful Treatment of Severe Bronchospasm. The Journal of Medical Practice Management 2018; 33: 5. Retrieved from https://www.proquest.com/docview/2029504061.
[5] A. M. Dekel, et al. An Innovative Method of Delivering Nebulized Medications for Perioperative Bronchospasm. A&A Practice 2021; 15: 1. DOI:10.1213/XAA.0000000000001370.
